
Migraines are severe, recurring headaches often accompanied by nausea, light sensitivity, and visual disturbances. Upper cervical chiropractic care addresses migraines by correcting misalignments in the atlas (C1) and axis (C2) vertebrae that can irritate the brainstem and trigeminal nerve—a primary pathway involved in migraine pain. Research shows 85-90% of migraine patients experience significant reduction in frequency and intensity with upper cervical care, often within 1-3 months.
Key Facts About Migraines
By downloading the Digital Patient Chart mobile app you can better control your patient portal.
- Affects: 39 million Americans (12% of the population); globally, 1 billion people
- Who ranking: 6th most disabling illness worldwide
- Treatment success: Studies show 85-90% improvement with upper cervical care
- Recovery timeline: Most patients notice improvement within 4-8 weeks
- Gender ratio: Women are 3x more likely to suffer migraines than men
- Specialist type: Upper cervical chiropractor (Blair Technique specialist recommended)
Medical Disclaimer: This content is for informational purposes only and does not constitute medical advice. The information provided should not be used for diagnosing or treating health problems or diseases. Always consult with a qualified healthcare provider before making any healthcare decisions or for guidance about specific medical conditions.
What Is a Migraine?
A migraine is far more than just a bad headache. It's a complex neurological condition that causes intense, often debilitating pain, typically on one side of the head, along with a constellation of other symptoms that can make normal functioning impossible.
The World Health Organization ranks migraines as the sixth most disabling illness in the world, comparable to dementia and quadriplegia in terms of years lost to disability. For the approximately 39 million Americans who suffer from migraines, this ranking makes perfect sense, attacks can leave you bedridden in a dark room for hours or even days.
Types of Migraines
Not all migraines are the same. Understanding your type helps determine the best treatment approach:
- Migraine Without Aura (Common Migraine): The most prevalent type, accounting for 70-80% of cases. Characterized by moderate to severe throbbing pain, typically on one side of the head.
- Migraine With Aura (Classic Migraine): Preceded by visual disturbances, numbness, tingling, or speech changes 20-60 minutes before headache onset.
- Vestibular Migraine: Features vertigo, dizziness, and balance problems as primary symptoms. Headache may be absent or mild.
- Chronic Migraine: Defined as 15 or more headache days per month, with at least 8 having migraine features. Severely impacts quality of life.
- Hemiplegic Migraine: A rare type causing temporary paralysis or weakness on one side of the body, along with visual disturbances.
- Menstrual Migraine: Occurs in relation to the menstrual cycle, typically in the days before, during, or after menstruation.
What Causes Migraines?
Scientists now understand migraines as a neurological disorder involving overactive nerve cells and changes in brain chemistry. While the exact cause isn't fully understood, we know migraines result from a complex interaction between genetics, brain chemistry, and environmental triggers.
The Trigeminal Nerve Connection
Current research points to the trigeminal nerve, the largest cranial nerve responsible for sensation in your face and head, as a primary player in migraine pain. When activated, this nerve releases inflammatory chemicals like calcitonin gene-related peptide (CGRP) and substance P, which cause blood vessels in the brain's protective membranes to swell and become inflamed.
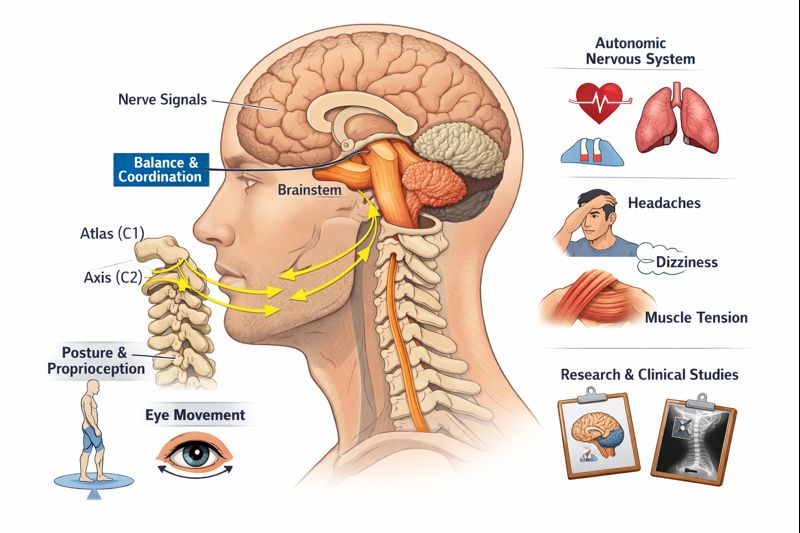
Here's the critical connection: The trigeminal nerve nucleus extends down into the upper cervical spine, directly adjacent to the atlas (C1) and axis (C2) vertebrae. When these vertebrae are misaligned, they can irritate and sensitize this nerve pathway, making migraine attacks more frequent and severe.
The Upper Cervical Connection
Research increasingly supports the role of upper cervical dysfunction in migraines. When the atlas or axis becomes misaligned, even by fractions of a millimeter, several migraine-promoting effects occur:
- Brainstem Irritation: The brainstem, which sits directly at the craniocervical junction, controls pain processing and blood vessel regulation. Misalignment can create pressure or tension affecting these functions.
- Trigeminal Nerve Sensitization: The trigeminal nucleus extends into the upper cervical area. Misalignment can irritate this pathway, lowering the threshold for migraine activation.
- Blood Flow Disruption: Vertebral arteries pass through the upper cervical vertebrae. Misalignment can affect blood flow to brain regions involved in migraine.
- CSF Flow Impairment: Recent research suggests upper cervical misalignment can impede cerebrospinal fluid drainage, potentially increasing intracranial pressure.
- Muscle Tension Patterns: Cervical misalignment creates chronic muscle tension in the neck and head, a well-known migraine trigger.
Common Migraine Triggers
Triggers don't cause migraines but can initiate an attack in susceptible individuals:
- Hormonal changes: Menstruation, pregnancy, menopause, birth control
- Dietary factors: Alcohol (especially red wine), aged cheeses, MSG, artificial sweeteners, skipping meals
- Environmental: Bright or flickering lights, strong smells, weather changes, high altitude
- Lifestyle: Stress (or stress letdown), sleep disruption, dehydration, intense physical exertion
- Physical: Neck pain, poor posture, jaw clenching, head or neck injury
Signs and Symptoms of Migraines
Migraines typically progress through distinct phases, though not everyone experiences all of them:
Phase 1: Prodrome (Hours to Days Before)
- Mood changes (depression, irritability, euphoria)
- Food cravings
- Neck stiffness
- Increased urination
- Yawning
- Fatigue
Phase 2: Aura (When Present, 20-60 Minutes Before)
- Visual disturbances (flashing lights, zigzag lines, blind spots)
- Numbness or tingling in face, arm, or leg
- Difficulty speaking
- Weakness on one side
- Ringing in ears
Phase 3: Attack (4-72 Hours)
- Intense, throbbing head pain (usually one-sided)
- Nausea and/or vomiting
- Extreme sensitivity to light (photophobia)
- Extreme sensitivity to sound (phonophobia)
- Sensitivity to smell
- Worsening with physical activity
Phase 4: Postdrome ("Migraine Hangover")
- Fatigue, exhaustion
- Difficulty concentrating
- Mood changes
- Weakness
- Residual head sensitivity
SEEK IMMEDIATE MEDICAL ATTENTION IF YOU EXPERIENCE:
- "Thunderclap" headache—severe pain reaching maximum intensity within seconds
- Worst headache of your life (different from usual migraines)
- Headache with fever, stiff neck, confusion, or seizures
- Headache after head injury
- New headache after age 50
- Headache with numbness, weakness, vision loss, or trouble speaking (stroke symptoms)
- Progressive headache that worsens over days/weeks
These may indicate stroke, aneurysm, meningitis, or other life-threatening conditions requiring emergency care.
How Are Migraines Diagnosed?
Migraine diagnosis is primarily clinical, based on your symptoms and medical history. A comprehensive evaluation typically includes:
Medical History & Symptom Review
Your healthcare provider will ask detailed questions about headache characteristics (location, quality, duration), frequency and timing, associated symptoms (nausea, sensitivity), triggers you've identified, family history of migraines, medications tried, and impact on daily life.
Diagnostic Criteria (ICHD-3)
According to International Classification of Headache Disorders, migraine without aura requires at least 5 attacks lasting 4-72 hours with at least 2 of these pain characteristics (one-sided, pulsating, moderate-to-severe intensity, worsened by activity) and at least 1 associated symptom (nausea/vomiting or light and sound sensitivity).
Upper Cervical Evaluation
A Blair Technique upper cervical chiropractor conducts specialized testing including:
- 3D CBCT Imaging: Cone Beam Computed Tomography reveals the precise position and angle of misalignment in the craniocervical junction
- Paraspinal Thermography: Measures temperature differences along the spine indicating nerve interference patterns
- Postural Analysis: Identifies head tilt, shoulder imbalance, and compensatory patterns
- Range of Motion Testing: Evaluates cervical spine mobility and restrictions
- Neurological Screening: Assesses cranial nerve function, reflexes, and coordination
The Blair Upper Cervical Technique for Migraines
The Blair Technique has shown remarkable success with migraine patients because it directly addresses one of the most common, and commonly overlooked, contributors to migraine: upper cervical misalignment.
How Blair Technique Works:
- Precision Imaging: 3D CBCT scans reveal the exact angle and direction of atlas/axis misalignment unique to your anatomy
- Gentle Adjustment: Light pressure (2-3 pounds of force) is applied in the precise direction needed, no twisting, cracking, or rotation
- Nervous System Restoration: Correcting alignment removes irritation to the brainstem and trigeminal pathways
- Holding Corrections: The goal is for adjustments to hold, reducing frequency of care over time
Research Support:
A study published in BioMed Research International following migraine patients who received upper cervical care found statistically significant improvement in migraine symptoms, including reduced frequency, intensity, and duration. Multiple case studies have documented complete resolution of chronic migraines following upper cervical correction.
Living With Migraines: Management Strategies
While pursuing treatment, these strategies can help reduce migraine frequency and manage attacks:
During an Attack
- Move to a dark, quiet room
- Apply cold compress to forehead or neck
- Stay hydrated with small sips of water
- Try to sleep if possible
- Practice deep, slow breathing
- Take acute medication early if prescribed
Lifestyle Modifications
- Maintain Regular Sleep: Go to bed and wake at consistent times, even on weekends
- Stay Hydrated: Dehydration is a common trigger—aim for 8+ glasses of water daily
- Don't Skip Meals: Blood sugar drops can trigger attacks
- Manage Stress: Practice relaxation techniques, mindfulness, or yoga
- Exercise Regularly: Moderate, consistent exercise helps—avoid intense bursts
- Limit Caffeine: Keep intake consistent; sudden changes can trigger attacks
- Watch Your Posture: Keep your head balanced over your shoulders, especially with screens
Keep a Migraine Diary
Track your attacks to identify patterns and triggers. Record date and time, what you ate and drank, sleep quality, stress level, weather, menstrual cycle (if applicable), prodrome symptoms, attack details (location, severity, duration), and what helped.
Prevention Strategies
Preventing migraines requires a multi-faceted approach:
- Regular Upper Cervical Care: Maintaining proper alignment prevents the neurological irritation that can trigger migraines
- Identify and Avoid Triggers: Use your migraine diary to recognize personal triggers
- Address Posture: Poor posture stresses the cervical spine—especially forward head position from device use
- Prompt Injury Treatment: Whiplash and head injuries often precede chronic migraines by months or years, get evaluated early
- Consider Supplements: Evidence supports magnesium, riboflavin (B2), and CoQ10 for some patients (discuss with provider)
When to See a Doctor
Schedule an appointment with a healthcare provider or upper cervical chiropractor if you experience:
- Migraines more than twice a month
- Headaches requiring frequent pain medication
- Migraines interfering with work, relationships, or quality of life
- Neck pain or stiffness accompanying headaches
- Migraines that started after a head or neck injury
- Medications that are no longer working or causing side effects
- New or changing headache patterns
Frequently Asked Questions
1. Can a chiropractor really help with migraines?
Yes—particularly upper cervical chiropractors who specialize in the relationship between the upper neck and nervous system. Research shows that many migraines involve dysfunction in the upper cervical spine, where the trigeminal nerve pathway, the primary pain pathway for migraines, extends. Correcting atlas and axis misalignment can reduce brainstem irritation and normalize nerve function, leading to fewer and less severe migraines. Studies show 85-90% of patients experience significant improvement.
2. How long does it take to see results?
Most patients begin noticing improvement within 4-8 weeks of starting care. Some experience significant relief after their first few adjustments, while others with long-standing migraines may need 2-3 months to see meaningful change. The duration of your condition, severity of misalignment, and how well your body holds corrections all influence your timeline. Many patients continue to improve over 6-12 months of care.
3. Is upper cervical chiropractic safe for migraines?
Upper cervical chiropractic care is extremely safe when performed by a trained specialist. The Blair Technique uses very gentle force—typically 2-3 pounds of pressure—without any twisting, rotation, or "cracking" of the neck. This precision approach, guided by 3D imaging, makes it one of the safest forms of spinal care available. The most common side effect is mild soreness that resolves within 24-48 hours. Serious adverse events are exceptionally rare.
4. What's the difference between a migraine and a regular headache?
Migraines are neurological events with distinct characteristics that differentiate them from tension or other headaches. Migraines typically feature throbbing or pulsing pain (often one-sided), moderate to severe intensity, associated symptoms like nausea and light/sound sensitivity, worsening with physical activity, and duration of 4-72 hours untreated. Regular tension headaches usually cause mild to moderate bilateral pressure, without nausea or significant sensitivity, and don't worsen with movement.
5. Can neck problems cause migraines?
Absolutely. The connection between neck problems and migraines is well-established. Cervicogenic headaches originate directly from neck dysfunction and can trigger or mimic migraines. More importantly, upper cervical misalignment can sensitize the trigeminal nerve pathway that's central to migraine pain, lower the threshold for migraine activation, create chronic muscle tension that triggers attacks, and affect blood flow and cerebrospinal fluid dynamics. Many people with chronic migraines trace their onset to a neck injury, whiplash, or concussion.
6. Will I need to take medication forever?
Not necessarily. Many migraine patients are able to reduce or eliminate medication use after addressing underlying upper cervical dysfunction. When the neurological irritation contributing to migraines is corrected, the need for medication often decreases. However, this should always be discussed with your prescribing physician, never stop or reduce medications without medical guidance. Some patients continue a combined approach, while others achieve full relief through upper cervical care alone.
7. How do I know if my migraines are related to my neck?
Signs that your migraines may have a cervical component include: migraines that started after a head or neck injury; neck pain, stiffness, or tenderness accompanying headaches; headaches that start at the base of the skull and radiate forward; attacks triggered by neck movements or sustained positions; migraines that haven't responded well to medication; and a history of whiplash, concussion, or poor posture. A comprehensive upper cervical evaluation can determine if spinal misalignment is contributing to your condition.
Ready to Take the Next Step?
Schedule a consultation at UC Spine Care to determine if upper cervical chiropractic can help your migraines.
Visit our website
The Bottom Line
Migraines are more than headaches, they're a neurological condition that can steal days, weeks, and years from your life. While medications can help manage symptoms, they don't address the underlying dysfunction that may be triggering your attacks.
For millions of migraine sufferers, that underlying dysfunction lies in the upper cervical spine. When the atlas and axis vertebrae are misaligned, they can irritate the brainstem and trigeminal nerve pathways central to migraine pain. The Blair Technique offers a precise, gentle way to correct these misalignments, without drugs, without surgery, and without the twisting or cracking of traditional chiropractic.
If you've been living with migraines, especially if they started after an injury, occur with neck symptoms, or haven't responded to other treatments, an upper cervical evaluation may reveal a correctable cause that's been missed. The first step is a comprehensive consultation to determine if this approach is right for you.
Key Takeaways
Migraines are neurological events involving the brainstem and trigeminal nerve—both intimately connected to the upper cervical spine
Upper cervical misalignment can sensitize migraine pathways, lowering your threshold for attacks
The Blair Technique uses precise, gentle adjustments—no twisting or cracking—to restore proper alignment
Research shows 85-90% of patients experience significant improvement with upper cervical care
Seek emergency care for thunderclap headache, worst headache ever, or headache with neurological symptoms
References
Woodfield HC, et al. (2015). Effect of atlas vertebrae realignment in subjects with migraine: an observational pilot study. BioMed Research International.
Elster EL. (2004). Upper cervical chiropractic care for a patient with chronic migraine headaches. Journal of Vertebral Subluxation Research.
Chaibi A, et al. (2017). Chiropractic spinal manipulative therapy for migraine: a single-blinded placebo-controlled trial. European Journal of Neurology.
Ashina M. (2020). Migraine. New England Journal of Medicine.
Bryans R, et al. (2011). Evidence-based guidelines for the chiropractic treatment of adults with headache. Journal of Manipulative and Physiological Therapeutics.
Headache Classification Committee of IHS. (2018). International Classification of Headache Disorders, 3rd edition. Cephalalgia.
American Migraine Foundation. (2024). Migraine Facts and Statistics. AMF Resources.
Burch RC, et al. (2021). The prevalence and impact of migraine and severe headache in the United States. Headache.
Goadsby PJ, et al. (2017). Pathophysiology of migraine: a disorder of sensory processing.
Physiological Reviews.
Haas M, et al. (2018). Dose-response and efficacy of spinal manipulation for cervicogenic headache. The Spine Journal.
Last medically reviewed: January 2026
Written by: UC Spine Care Medical Content Team






Leave a comment