
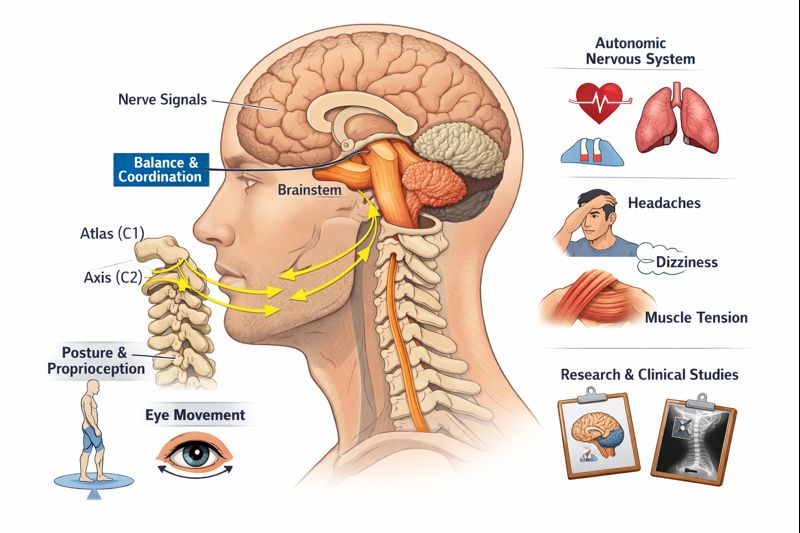
Cervicogenic dizziness is a condition where neck problems cause feelings of unsteadiness, disorientation, and imbalance. Unlike true vertigo, which creates a spinning sensation from inner ear problems, cervicogenic dizziness stems from dysfunction in the cervical spine, particularly the upper neck region where the atlas (C1) and axis (C2) vertebrae connect to the skull. Approximately 75% of patients experience significant improvement with proper cervical spine treatment, including upper cervical chiropractic care.
Key Facts
By downloading the Digital Patient Chart mobile app you can better control your patient portal.
- Prevalence: Affects 20-50% of people with chronic neck pain
- Common Causes: Whiplash injuries, poor posture, cervical misalignment, degenerative changes
- Typical Duration: Symptoms last minutes to hours, often worsening with head movements
- Treatment Success Rate: 75% improve with conservative neck treatment
- Specialist Type: Upper cervical chiropractor, vestibular therapist, or neurologist
Medical Disclaimer: This content is for informational purposes only and does not constitute medical advice. The information provided should not be used for diagnosing or treating health problems or diseases. Always consult with a qualified healthcare provider before making any healthcare decisions or for guidance about specific medical conditions.
What Is Cervicogenic Dizziness?
Cervicogenic dizziness (CGD) is a syndrome characterized by dizziness and imbalance that originates from problems in the cervical spine rather than the inner ear or brain. The term "cervicogenic" literally means "arising from the neck," distinguishing this condition from vestibular disorders that affect the balance organs in your inner ear.
People with cervicogenic dizziness typically describe their symptoms differently than those with true vertigo. Instead of feeling like the room is spinning, they often experience a floating sensation, lightheadedness, or a general sense of disorientation. These symptoms are closely tied to neck position and movement—turning your head, looking up, or maintaining certain postures can trigger or worsen the dizziness.
The condition involves a complex interplay between your cervical spine and your brain's balance centers. Your upper neck contains an extremely high concentration of proprioceptors—specialized nerve sensors that tell your brain where your head is positioned in space.
When the cervical spine is misaligned or dysfunctional, these proprioceptors send conflicting signals to the brain, creating a "sensory mismatch" between what your neck senses, what your eyes see, and what your inner ear detects.
This sensory mismatch confuses your brain's balance processing centers, resulting in the characteristic dizziness and unsteadiness of cervicogenic dizziness.
What Causes Cervicogenic Dizziness?
Cervicogenic dizziness develops when something disrupts the normal function of your cervical spine or the nerves and blood vessels that pass through it. Understanding these causes is essential for effective treatment.
1. Traumatic Injury
Whiplash from car accidents is the most commonly identified cause of cervicogenic dizziness. The sudden acceleration-deceleration forces can damage soft tissues, misalign vertebrae, and injure the proprioceptive nerve endings in your neck. Studies show that 40-85% of whiplash patients develop some form of dizziness following their injury.
2. Upper Cervical Misalignment
The atlas (C1) and axis (C2) vertebrae at the top of your neck are uniquely vulnerable to misalignment. Unlike other vertebrae, they lack interlocking joints and rely primarily on ligaments and muscles for stability.
Even subtle misalignments in this region, sometimes measuring just millimeters—can compress nerves, restrict blood flow through the vertebral arteries, and disrupt proprioceptive signaling.
3. Degenerative Changes
Cervical spondylosis, disc degeneration, and arthritis can alter the mechanics of your neck and irritate the nerve-rich structures surrounding your spine. As degenerative changes progress, abnormal bone growth and disc bulging may further compromise nerve function and blood flow.
4. Muscle Dysfunction
Chronic tension, trigger points, and weakness in the deep neck stabilizer muscles can alter proprioceptive input from the cervical spine. Poor posture habits, prolonged screen use, and occupational stressors often contribute to this muscle dysfunction.
Risk Factors
Several factors increase your likelihood of developing cervicogenic dizziness:
- History of neck or head trauma
- Chronic neck pain or stiffness
- Forward head posture (common in office workers)
- Previous concussion
- Cervical spine surgery
- Age-related degenerative changes
- Signs and Symptoms {#symptoms}
Cervicogenic dizziness presents with a distinct pattern of symptoms that differentiate it from other causes of dizziness. Recognizing these characteristics helps ensure accurate diagnosis and appropriate treatment.
Primary Symptoms
The hallmark symptoms of cervicogenic dizziness include:
1. Dizziness with neck movement: Symptoms typically worsen when you turn your head, look up, or maintain certain neck positions for extended periods. This movement-related pattern distinguishes CGD from many other dizziness disorders.
2. Non-spinning sensation: Rather than the rotational vertigo typical of inner ear problems, cervicogenic dizziness usually produces a sensation of floating, unsteadiness, or general disorientation. Some describe it as feeling "off" or like walking on uneven ground.
3. Concurrent neck symptoms: Neck pain, stiffness, and reduced range of motion frequently accompany the dizziness. The dizziness often improves as neck symptoms improve.
4. Duration of episodes: Symptoms typically last minutes to hours, though some people experience more persistent, lower-grade dizziness throughout the day.
Associated Symptoms
Many people with cervicogenic dizziness also experience:
- Headaches, particularly at the base of the skull (occipital headaches)
- Visual disturbances during head movements
- Difficulty concentrating or "brain fog"
- Nausea (usually milder than with vestibular vertigo)
- General imbalance, especially when walking
- Anxiety related to dizziness episodes
- Ear fullness or tinnitus (ringing in the ears)
Symptom Patterns
Symptoms of cervicogenic dizziness tend to follow predictable patterns. They often worsen with activities requiring neck movement or sustained postures—such as driving, working at a computer, or looking over your shoulder. Conversely, symptoms may improve with rest or when the neck is in a neutral, supported position.
SEEK IMMEDIATE MEDICAL ATTENTION IF YOU EXPERIENCE:
- Sudden, severe dizziness with difficulty speaking or understanding speech
- Dizziness accompanied by sudden severe headache
- Loss of consciousness or fainting
- Double vision or sudden vision loss
- Difficulty walking, loss of coordination, or falling
- Numbness or weakness, especially on one side of the body
- Dizziness following a significant head or neck injury
These symptoms may indicate stroke, concussion, or other serious conditions requiring emergency care.
How Is Cervicogenic Dizziness Diagnosed?
Diagnosing cervicogenic dizziness requires a systematic approach because no single test can definitively confirm the condition. Healthcare providers must first rule out other causes of dizziness—particularly vestibular disorders and central nervous system problems—before arriving at a cervicogenic diagnosis.
Clinical Evaluation
Your provider will conduct a thorough history and physical examination, including:
- Detailed symptom history: Documenting when your dizziness started, what triggers or worsens it, how long episodes last, and whether neck pain accompanies your symptoms.
- Neck examination: Assessing cervical range of motion, identifying tender or restricted areas, and evaluating muscle tension and function.
- Neurological testing: Checking reflexes, sensation, strength, and coordination to rule out central nervous system involvement.
- Vestibular testing: Performing specific tests like the Dix-Hallpike maneuver to evaluate for benign paroxysmal positional vertigo (BPPV) and other vestibular conditions.
- Specialized Tests
Several clinical tests help identify cervicogenic contributions to dizziness: - Cervical torsion test: Assessing whether rotating your trunk while keeping your head still reproduces dizziness symptoms. A positive result suggests cervical involvement.
- Smooth pursuit neck torsion test: Evaluating eye movement control with the neck in different positions. This test shows high specificity (around 91%) for cervicogenic dizziness.
- Joint position error testing: Measuring how accurately you can return your head to a target position with eyes closed. Increased error suggests impaired cervical proprioception.
Imaging Studies
While not always necessary, imaging may include:
- X-rays: Evaluating spinal alignment and identifying degenerative changes
- 3D Cone Beam CT: Providing detailed visualization of upper cervical anatomy, particularly useful for Blair Upper Cervical practitioners
- MRI: Ruling out disc herniations, tumors, or other soft tissue problems
Cervicogenic dizziness is ultimately a "diagnosis of exclusion"—meaning other causes must be ruled out first. This process ensures that potentially serious conditions aren't missed while confirming that the cervical spine is the primary driver of your symptoms.
Treatment Options
Treatment for cervicogenic dizziness focuses on restoring normal cervical spine function, improving proprioceptive accuracy, and retraining your balance system. The most effective approach often combines multiple treatment modalities.
Upper Cervical Chiropractic Care
Upper cervical chiropractic care specifically targets the atlas and axis vertebrae—the region most commonly implicated in cervicogenic dizziness. The Blair Upper Cervical Technique is particularly well-suited for this condition.
How Blair Upper Cervical Care Works:
The Blair technique uses precision 3D imaging to identify the exact nature and direction of upper cervical misalignments. Unlike general chiropractic manipulation, Blair adjustments are:
- Highly specific to each patient's unique anatomy
- Gentle with no twisting, popping, or cracking of the neck
- Targeted precisely to address the identified misalignment
- Designed to restore proper nerve function and blood flow
Research published in the Journal of Chiropractic Medicine and other peer-reviewed publications has documented improvements in dizziness symptoms following upper cervical adjustments. By correcting atlas and axis misalignments, upper cervical care addresses potential root causes of cervicogenic dizziness, including nerve interference near the brainstem, vertebral artery compromise, and disrupted proprioceptive signaling.
Living With Cervicogenic Dizziness
While seeking treatment for cervicogenic dizziness, there are steps you can take to manage symptoms and support your recovery.
Daily Management Strategies
Posture awareness: Maintaining good posture reduces strain on your cervical spine. Keep your ears aligned over your shoulders and avoid prolonged forward head positions. Set reminders to check your posture throughout the day, especially if you work at a computer.
Movement modifications: If certain movements trigger your dizziness, modify activities temporarily. Turn your whole body rather than just your head when possible, and avoid sudden head movements until symptoms improve.
Workspace ergonomics: Position your computer monitor at eye level, use a headset for phone calls, and ensure proper keyboard and mouse placement to reduce neck strain.
Sleep positioning: Use a supportive pillow that maintains neutral neck alignment. Avoid sleeping on your stomach, which forces your neck into rotation.
Lifestyle Considerations
Stress management: Stress and anxiety can worsen cervicogenic dizziness by increasing muscle tension. Practices like deep breathing, meditation, and gentle yoga may help reduce symptoms.
Activity pacing: Balance rest with gentle activity. While avoiding all movement can actually worsen symptoms, pushing through severe dizziness isn't helpful either.
Hydration and nutrition: Dehydration can worsen dizziness. Maintain adequate fluid intake and eat regular, balanced meals.
Emotional Support
Living with dizziness can be emotionally challenging. The unpredictability of symptoms may lead to anxiety, frustration, or social withdrawal. Remember that cervicogenic dizziness is a real, recognized condition with effective treatments.
Connecting with others who understand your experience—whether through support groups or open communication with loved ones—can make the journey easier.
Prevention Strategies
While not all cases of cervicogenic dizziness can be prevented, you can reduce your risk and potentially prevent recurrence:
Maintain good posture: Especially important in our digital age. Regular posture checks and ergonomic workstation setup can protect your cervical spine.
Exercise regularly: Strength training, flexibility work, and cardiovascular exercise all support spine health. Focus on neck and upper back strengthening exercises.
Address neck problems early: Don't ignore persistent neck pain or stiffness. Early intervention may prevent progression to cervicogenic dizziness.
Protect yourself from injury: Use proper seatbelt positioning, headrest adjustment, and protective equipment during sports to reduce whiplash and head injury risk.
Take movement breaks: If you have a sedentary job, stand up and move every 30-60 minutes. Gentle neck stretches and shoulder rolls can help maintain mobility.
When to See a Doctor
Seek professional evaluation if you experience:
- Dizziness lasting more than a few days
- Dizziness accompanied by neck pain or stiffness
- Dizziness that worsens with head or neck movement
- Previous neck or head injury with new dizziness symptoms
- Dizziness affecting your ability to work, drive, or perform daily activities
Any "red flag" symptoms listed in the emergency section above. Early evaluation and treatment typically lead to better outcomes. Don't wait for symptoms to become severe or chronic before seeking help.
Frequently Asked Questions
1. What's the difference between cervicogenic dizziness and vertigo?
True vertigo creates a spinning sensation—either you feel like you're spinning or the room is spinning around you—and typically originates from inner ear problems. Cervicogenic dizziness produces a different sensation: unsteadiness, lightheadedness, or disorientation without the spinning component.
Cervicogenic dizziness comes from the neck and is strongly associated with neck movement and positioning. However, some people use "vertigo" loosely to describe any dizziness, which can create confusion. Proper diagnosis requires differentiating between these distinct conditions.
2. Can upper cervical chiropractic care help with my dizziness?
Upper cervical chiropractic care can be highly effective for cervicogenic dizziness, particularly when neck misalignment contributes to your symptoms. The Blair Upper Cervical Technique specifically addresses the atlas and axis vertebrae, the spinal segments most commonly associated with cervicogenic dizziness.
By restoring proper alignment and function to this critical region, upper cervical care may improve proprioceptive signaling, relieve nerve interference, and optimize blood flow through the vertebral arteries. Many patients experience significant improvement, though individual results vary based on the underlying cause and severity of dysfunction.
3. How long does cervicogenic dizziness take to heal?
Recovery time varies considerably depending on the cause and severity of your condition, how long you've had symptoms, and your response to treatment. Some patients notice improvement within a few treatment sessions, while others require several months of consistent care.
Research indicates that approximately 75% of patients with cervicogenic dizziness improve with appropriate treatment. Chronic cases or those involving multiple contributing factors may take longer to resolve. Your healthcare provider can give you a more personalized timeline based on your specific situation.
4. Is cervicogenic dizziness permanent?
Cervicogenic dizziness is not typically permanent. With proper treatment addressing the underlying cervical dysfunction, most patients experience significant improvement or complete resolution of symptoms. However, without treatment, symptoms may persist or worsen over time.
In some cases, particularly when dizziness follows whiplash or other trauma, symptoms may fluctuate or recur with stress, poor posture, or overexertion, even after initial improvement. Ongoing maintenance care and attention to prevention strategies can help maintain long-term relief.
5. Can poor posture really cause dizziness?
Yes, poor posture can contribute to cervicogenic dizziness. Forward head posture—common in people who spend hours at computers or looking at phones—places significant strain on the cervical spine and its supporting structures.
This altered positioning can affect proprioceptive signaling from the neck, contribute to muscle imbalances, and potentially compromise blood flow through the vertebral arteries. Over time, these effects may result in dizziness symptoms. Correcting postural habits is often an important component of treatment and prevention.
6. Should I be worried about my cervicogenic dizziness?
While cervicogenic dizziness itself is not dangerous, it's important to have your symptoms properly evaluated. Dizziness has many potential causes, and some, though rare, can be serious. The evaluation process rules out concerning conditions like stroke, tumors, or significant vestibular disorders.
Once cervicogenic dizziness is confirmed, you can feel reassured that effective treatments exist. The symptoms may be unpleasant and disruptive, but they are typically very treatable with appropriate care. If you experience any "red flag" symptoms listed earlier in this article, seek immediate medical attention.
7. How is cervicogenic dizziness different from Meniere's disease?
Meniere's disease is a vestibular disorder affecting the inner ear, characterized by episodes of spinning vertigo, fluctuating hearing loss, tinnitus (ringing in the ear), and a feeling of fullness in the affected ear. Episodes typically last 20 minutes to several hours.
Cervicogenic dizziness, in contrast, originates from the neck, doesn't affect hearing, and produces unsteadiness rather than spinning vertigo. The key distinguishing factor is the relationship with neck movement and positioning, cervicogenic dizziness symptoms clearly correlate with cervical spine position and movement, while Meniere's episodes occur more unpredictably.
Ready to Take the Next Step?
If you're experiencing dizziness related to neck problems, upper cervical chiropractic care may provide the relief you're seeking. The Blair Upper Cervical Technique offers a precise, gentle approach specifically designed to address the upper cervical spine, the region most commonly associated with cervicogenic dizziness.
UC Spine Care specializes in Blair Upper Cervical Chiropractic care for patients throughout Los Angeles and the greater Southern California area.
Trust your instincts. If you're concerned about your symptoms, it's always appropriate to seek professional evaluation and guidance.
Cervicogenic dizziness is a real and treatable condition that connects neck dysfunction to symptoms of dizziness, unsteadiness, and disorientation. Unlike inner ear disorders that cause spinning vertigo, cervicogenic dizziness stems from problems in the cervical spine—particularly the upper neck region where the atlas and axis vertebrae are located.
The good news is that approximately 75% of people with cervicogenic dizziness experience improvement with appropriate treatment. Upper cervical chiropractic care, particularly the Blair Technique, offers a precise, gentle approach to addressing the root cause of many cervicogenic dizziness cases.
By restoring proper alignment and function to the upper cervical spine, this specialized care can help relieve nerve interference, improve proprioceptive signaling, and optimize blood flow to the brain.
If you've been experiencing dizziness along with neck symptoms, especially if your dizziness relates to head movement or positioning, cervicogenic causes should be considered. Don't settle for a life disrupted by dizziness when effective treatment options exist. Seek evaluation from a qualified provider who can accurately diagnose your condition and develop a personalized treatment plan to help you find lasting relief.
References
Furman JM, Cass SP. Balance Disorders: A Case-Study Approach. Philadelphia: F.A. Davis; 1996. Definition of cervicogenic dizziness.
Wrisley DM, Sparto PJ, Whitney SL, Furman JM. Cervicogenic dizziness: a review of diagnosis and treatment. J Orthop Sports Phys Ther. 2000;30(12):755-766.
Vestibular Disorders Association. Cervicogenic Dizziness. https://vestibular.org/article/diagnosis-treatment/types-of-vestibular-disorders/cervicogenic-dizziness/. Updated 2024.
Treleaven J. Sensorimotor disturbances in neck disorders affecting postural stability, head and eye movement control. Man Ther. 2008;13(1):2-11.
Devaraja K. Approach to cervicogenic dizziness: a comprehensive review of its aetiopathology and management. Eur Arch Otorhinolaryngol. 2018;275(10):2421-2433.
Lystad RP, Bell G, Bonnevie-Svendsen M, Carter CV. Manual therapy with and without vestibular rehabilitation for cervicogenic dizziness: a systematic review. Chiropr Man Therap. 2011;19(1):21.
Malmström EM, Karlberg M, Melander A, Magnusson M, Moritz U. Cervicogenic dizziness – musculoskeletal findings before and after treatment and long-term outcome. Disabil Rehabil. 2007;29(15):1193-1205.
Reid SA, Rivett DA, Katekar MG, Callister R. Comparison of mulligan sustained natural apophyseal glides and maitland mobilizations for treatment of cervicogenic dizziness: a randomized controlled trial. Phys Ther. 2014;94(4):466-476.
Physiopedia. Cervicogenic dizziness: screening. https://www.physio-pedia.com/Cervicogenic_dizziness:_screening. Accessed 2024.
Journal of Upper Cervical Chiropractic Research. Case studies on upper cervical care and vestibular symptoms. Multiple publications 2015-2023.
Last medically reviewed: November 2025
Written by: UC Spine Care Content Team






Leave a comment